- What conditions do they treat?
- What procedures do they do?
- How much do they earn?
- What is their lifestyle?
- How to become a cardiologist
- Typical career path
- Fellowship programs
- Additional resources
Cardiology is the study and treatment of disorders of the heart and the blood vessels. A person with heart disease or cardiovascular disease may be referred to a cardiologist.
What conditions do they treat?
Neurologists treat neurological conditions, which are problems that affect the brain, spinal cord, and nerves. These conditions include:
- stroke
- epilepsy
- headaches and migraines
- brain tumors
- brain aneurysms
- peripheral neuropathy
- sleep disorders
- neurodegenerative diseases, such as Parkinson’s disease and Alzheimer’s disease
- neuromuscular diseases, such as myasthenia gravis, multiple sclerosis (MS), and amyotrophic lateral sclerosis (ALS)
- infections of the nervous system, such as encephalitis, meningitis, and HIV
Neurologist procedures
Neurologists perform a range of different tests and procedures to diagnose and treat neurological conditions.
Some of these procedures include:
Lumbar puncture
A neurologist can use a lumbar puncture to collect a sample of spinal fluid. They may use this procedure to help diagnose the following conditions:
- meningitis
- encephalitis
- myelitis
- leukemia
- autoimmune diseases, such as multiple sclerosis (MS)
- dementia
- bleeding in the brain
Neurologists can also use a lumbar puncture to treat conditions that affect the spinal cord. They can inject anesthetics, antibiotics, or cancer treatments using a lumbar puncture needle.
Electromyography
A neurologist can use electromyography (EMG) to assess how well a person’s muscles respond to electrical stimulation from motor neurons, which are specialized nerves that control muscle movement.
During an EMG, a specially trained technician inserts small needles called electrodes into the muscle. These electrodes record the different electrical activity that occurs in muscle tissue during periods of movement and rest.
The EMG machine produces an electromyogram, which is a record of this activity.
Neurologists can use the results of an EMG to diagnose neuromuscular diseases, such as myasthenia gravis and ALS.
Electroencephalogram
Neurologists use electroencephalograms (EEG) to measure and record electrical activity in the brain. Neurons in the brain communicate with other neurons through electrical impulses, which an EEG can pick up. An EEG can also track brain wave patterns.
During an EEG, a technician will place electrodes on the person’s head. These electrodes connect to a computer that converts electrical signals into patterns that the technician can view on a screen or print on a piece of paper.
Neurologists can use EEG results to identify abnormal electrical activity in the brain and diagnose certain conditions, such as:
- epilepsy
- seizures
- brain tumors
- sleeping problems
Tensilon test
Myasthenia gravis is a rare neuromuscular disease that weakens the muscles in the arms and legs. A neurologist can use a blood test called a Tensilon test to diagnose myasthenia gravis.
Tensilon is the brand name of a drug called edrophonium, which prevents the breakdown of acetylcholine, a neurotransmitter that stimulates muscle movement. Myasthenia gravis causes the immune system to attack acetylcholine receptors in the muscles, which causes muscle fatigue and decreased muscle movement.
During a Tensilon test, a neurologist will inject a small amount of Tensilon into the bloodstream. Then, they will ask the person to perform different movements, such as:
- standing up and sitting down
- holding their arms above their head
- crossing and uncrossing their legs
The neurologist will continue administering doses of Tensilon each time the person feels tired. If the person notices that their strength returns after each Tensilon injection, this indicates that they are likely to have myasthenia gravis.
Other tests
A neurologist can use the following tests to help diagnose neurological disorders:
- laboratory tests, such as blood and urine analyses
- imaging tests, such as ultrasounds and MRI, CT, and PET scans
- genetic testing
- biopsy
- angiography
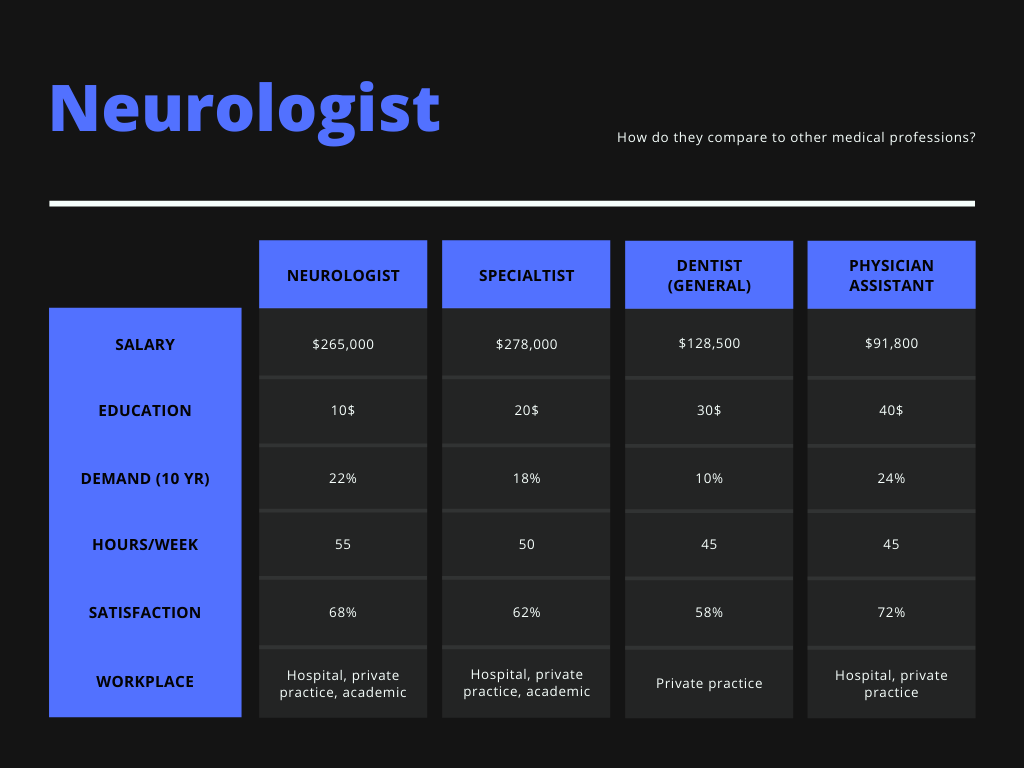
Neurologist salary
Since neurocritical care is a relatively new field, and relatively small, compensation data is not as thorough as it is for neurologists. However, according to the NCS, the median salary of a neurocritical care physician is within the range of $250,000–$300,000 USD.
Only 7% of respondents earned over $401,000 annually. The median salary for males was $276,000–$300,000, while for females, it was $251,000–$275,000 (Table 2).
The most common compensation model was receiving salary only (Fig. 1). Generally, the more an intensivist worked, the higher the pay. The median income for a physician working 26 or more weeks was $301,000–$325,000, while those working 13 weeks or less made a median income of $226,000–$250,000 (Fig. 1).
Across the USA, median incomes were similar except for the West with a higher median income of $301,000–$325,000 (Table 2).
As you might expect, private practice and multi-specialty group practices tended to earn more on average than the academic setting.
Midwest - $310,000
Northwest - $295,000
Neurology subspecialties
Common subspecialties of neurology include:
- pediatric or child neurology
- neurodevelopmental disabilities
- neuromuscular medicine
- hospice and palliative care neurology
- pain medicine
- headache medicine
- sleep medicine
- vascular neurology
- autonomic disorders
- neuropsychiatry
- brain injury medicine
- neurocritical care
- epilepsy
Neurology lifestyle
The median service weeks for academic faculty were 18–21 ICU weeks (Online Supplement). All other practice settings work a median 26 or more service weeks. Salary characteristics are further broken down in the Online Supplement.
Neurology vs. other professions
Neurologists on average earn slightly less than other specialists, but work less hours and are in higher demand over the next 10 years.
Neurology career paths
The vast majority of neurocritical care physicians are board-certified in neurology, and go on to pursue a fellowship in neurocritical care from an accredited program.
A small percentage of neurocritical care physicians are board-certified in urgent care or emergency medicine before being accepted into a neurocritical care fellowship program.
Most neurocritical care fellowships are 1 year.

Neurology fellowship programs
As neurocritical care is relatively new, there are just 10 accredited programs in the US as of February 2021.
- Stanford University Hospital Neurocritical Care Fellowship
- University of Michigan Hospital Neurocritical Care Fellowship
- University of Michigan Hospital Neurocritical Care Fellowship
- Stanford University Hospital Neurocritical Care Fellowship
- University of Michigan Hospital Neurocritical Care Fellowship
These programs are highly competitive. To stand out, having a strong background in neurological research or demonstrated interest in the field can help you land an interview.
Learn more about neurology
To learn more, visit these websites:
- Neurocritical Care Society (NCS)
Know a neurologist?
MedCareer would love to interview neurocritical care physicians to help aspiring physicians and medical students learn about your field!
Contact drew@medcareer.io if you are interested :)